The Devil’s Nectar: The Science Behind Alcohol
“Ah my Beloved, fill the Cup that clears
Today of past Regrets and future Fears.
Tomorrow? - Why, Tomorrow I may be
Myself with Yesterday’s Seven Thousand Years”
XX Rubaiyat of Omar Khayyam, 12th Century
Strange Brew
Alcohol is the most widely consumed psychotropic substance in the world. A cultural history of alcohol would fill a library and the scientific literature is similar in volume. In countries where alcohol is legal one is never too far away from a cold beer or other enticing beverage. Most adults have a pretty clear idea of the effects of alcohol. Yet, in getting to the bottom of fairly simple questions like what exactly alcohol does to the body, how does the body process it, or how much is okay to drink regularly before it starts damaging health, it can be quite hard to pin down precise answers.
Popular articles about alcohol tend to fall into three main types. Firstly, there is the simple ‘food and drink’ piece about the latest summer cocktail or best wine to pair with a beef Wellington which colourfully describes the flavours of a particular beverage but is somewhat coy about the key ingredient. Then there are the ‘Why I Gave Up Drinking’ confessionals in which the narrator describes a descent into dipsomania - hopefully with plenty of lurid detail - before an arduous climb to the sunny uplands of sobriety. More recently we have seen ‘this is what happened when I gave up alcohol’ piece in which the writer somewhat unsurprisingly reports better sleep, more energy, better skin and so on upon quitting drink. Then there is the third science-based ‘latest study’ type that promises to settle, once and for all, the question of whether moderate drinking is okay or bad for one’s health. The findings seem to change according to what day of the week it is and usually leave the reader none the wiser. To be fair on health reporters they have an uphill task picking apart the slew of conflicting research, and unlike personal stories which are relatable and easy to process, statistical data is tricky to get one’s head around. I for one am left groping for the drinks cabinet upon reading phrases like ‘Mendelian regression’ or ‘collider bias’.
Discussion about alcohol tends to be all-or-nothing; either booze-hell or sober-heaven, a habit which is either healthy or high-risk, and in Western culture there is often a slight whiff of morality when we talk about drink, as if - Heaven forbid - we should actually show people enjoying something without some consequence. Of the above mentioned types of article about alcohol, it is perhaps the food and drink ones which are the most useful: Not only are they guides on how to actually enjoy a drink, but they all implicitly contain a crucial piece of wisdom, backed by science, which we will come to shortly.
Alcohol: A Brief History
Alcohol, or ethanol, is a water soluble molecule that is most commonly produced in nature by fermented fruits. It is ingested by many species, including birds, bats, insects and apes, who primarily use it as a source of fuel (and possibly intoxicant). Its relevance to humans is that around 10 million years ago in pre-human hominids, there was a significant mutation in a gene that encodes an enzyme called ADH4 which is abundant in the upper GI tract (oesophagus, stomach and duodenum). This mutation resulted in a 40-fold increase in our ape-like ancestors’ capacity to metabolise alcohol and occurred around the same time that they were shifting down to terrestrial habitats. The upshot is that they were better able to tolerate ethanol in the fermented fruits abundant on the forest floor, which they could now use as an extra fuel source. This raises the interesting question of how far this new found ability to literally stomach alcohol contributed to our evolution to homo sapiens. In any case the fact that they were able to use fallen fruit as fuel was an important evolutionary bonus. Also, as no longer tree-dwelling their arms could be used for other things like manipulating tools etc. while they learned to walk on two legs, or stagger depending on the amount of ‘fruit’ they had consumed.
There is plenty of archaeological evidence of pre-historical alcohol use. In what is now the Middle East, the Natufian hunter-gatherers were brewing beer around 13000 BCE, while in Neolithic China around 7000 BCE beverages were being brewed from rice, honey and fruits. For the ancient Egyptians beer was a staple and there is compelling evidence that the Great Pyramids were constructed, not from alien technology, but good old-fashioned labour, with armies of workers supplied by vast canteens dishing out beer and beef-burgers (apparently). Wine was supped in Ancient Greece and Persia, including by the legendary mathematician Omar Khayyam whose famous poetry contains more than one mention of ‘The Grape’. In medieval Europe monks diversified as expert vintners and brewers and in Victorian Britain, before Bazalgette’s sewers revolutionised public health, it was far safer to drink ale than the London water, possibly accounting for the ubiquity of pubs in London.
Of course, for some cultures alcohol has been destructive. The white settlers in North America didn’t hesitate in encouraging alcohol use among the Native Americans, for whom alcohol remains a leading cause of premature death. Nor were these European immigrants immune. Jack London’s classic autobiography John Barleycorn: A Drinking Life, describes in vivid detail just how pickled many parts of the US were in the early 20th century, with bars and salons spilling out into every main street, and the widespread drunkenness - and no doubt fear about the productivity of the workforce - eventually culminating the policy of Prohibition. Throughout human history alcohol has been variously a fuel, a medicine, an intoxicant, a euphoriant, a ritual brew, a social lubricant, a culinary art and an agent of destruction.
The Physical and Mental Effects of Alcohol
The psychological and physical effects of alcohol are difficult to tell apart. Before the first drink touches our lips our brain is already releasing neurotransmitters like dopamine in anticipation. One of the characteristic features of alcohol dependency is ‘salience’ whereby an increasing proportion of one’s thoughts revolve around drink. For the drinker this can provoke all manner of emotions - shame, despair, anticipation, etc - yet is really, on an organic level, simply motivated by the nervous system seeking out alcohol to re-balance it. Likewise that vague sense of shame and guilt that often follows a big night out is, in the most part, due to imbalances in brain chemistry rather than any shocking behaviour the night before, or at least one hopes. Regardless of the varied mental, social and cultural effects of alcohol, the biological ‘mechanism of action’ is virtually the same for everyone.
Absorbtion
Once ingested, alcohol is absorbed in the lining of the upper GI tract and then processed via the liver before entering the rest of the body, via the systemic circulation. During its passage through the upper GI tract and liver it undergoes first pass metabolism (FPM) where, depending on conditions such as food in the stomach, as much as 25-50% of the alcohol is already processed before it even gets into the systemic circulation. The ethanol that makes it past FPM diffuses quickly through the bloodstream to the organs and tissues of the body, especially to those parts with a high blood supply relative to their mass, such as the liver, kidneys and brain. Alcohol is more slowly absorbed by muscle, though more muscle provides more ‘lean mass’ for distribution, leading to slower peak blood alcohol concentration (peak BAC). Alcohol is barely at all absorbed into fat. A slow peak BAC and faster elimination rate of alcohol is generally healthier with regards to alcohol consumption.
GABA and Glutamate
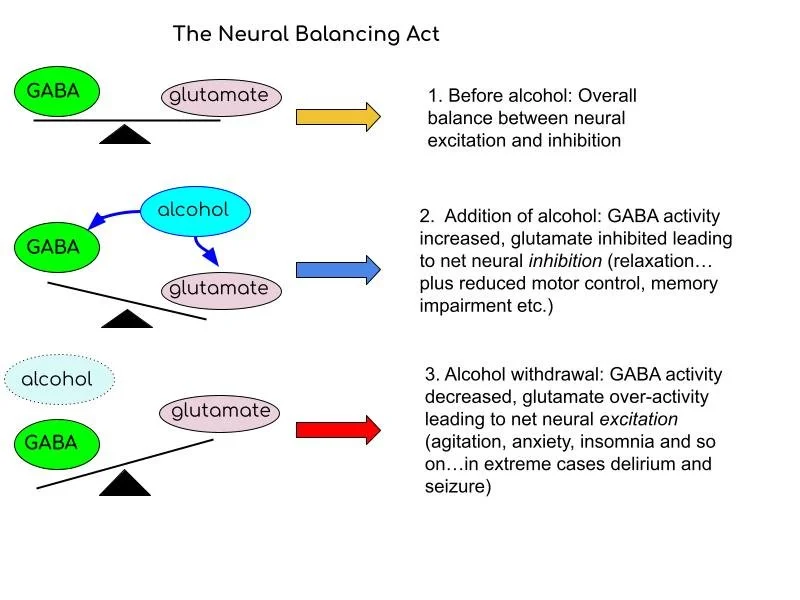
In the brain alcohol acts on a receptor abundant on the surface of neurons called the GABA-a receptor, normally activated by GABA (gamma amino butyric acid), the brain's major inhibitory neurotransmitter. Receptors can be thought of as doors on the cell surface, and neurotransmitters as keys, which allow certain molecules to flood into the cell, changing their activity. Alcohol both potentiates the GABA-a receptor, essentially supercharging it, and acts to release GABA itself, resulting in overall increased neural inhibition. Additionally, alcohol inhibits the excitatory neurotransmitter glutamate (which acts on a receptor called NMDA), further relaxing the nervous system. It also promotes the release of dopamine and serotonin, accounting for its euphoric and addictive qualities.
However, a common feature of human biology is that what goes up must come down and vice versa. With repeat exposure the body down-regulates GABA-a receptors, making them sparser on the cell surface, and up-regulates NMDA receptors. In the absence of alcohol, say the following day after a night out, or if a chronic drinker decides to stop suddenly, this essentially results in too little GABA and too much glutamate activity, leading to overall neural excitation. Glutamate is important in thinking, memory and learning, but too much of it, and too little GABA, leads to the agitation and anxiety of alcohol withdrawal, and can even lead to delirium tremens, seizure and worse. Alcohol also depletes vitamin B stores, in particular B1, aka thiamine, and this in turn can result in a condition called Wernicke's encephalopathy, characterised by confusion, imbalance, memory-loss and potential brain damage (Korsakoff's syndrome). It is for this reason that heavy drinkers should never go cold-turkey, no matter how well-intentioned, and ought to take regular B-vitamins.
Heavy Vs Moderate
The majority of drinkers never reach this stage. The figures vary by country, but globally around 4% of all drinkers develop an alcohol use disorder (AUD) at some time - a lot of people, but still a minority. It’s not entirely clear why some people are more prone than others. Genetic predisposition, social factors, personal history, exposure to drink and so on all play a role, and quite unpredictably, to the extent that it is pointless to blame the heavy drinker for developing an addiction. In any case most drinkers avoid this. Even if they were pretty hedonistic in their youth, excessive alcohol use is normally staved off in most by a combination of reduced tolerance to hangovers and bleary eyed mornings, burgeoning responsibilities, a vague post-alcohol guilt and, basically, reduced social opportunities for drinking. Some people take this as an opportunity to stop altogether, perhaps they never really enjoyed drinking anyway, and some simply don’t trust themselves to drink, perhaps finding it pulls them into oblivion a little too quickly.
On the other hand many people are not quite ready to say goodbye to alcohol just yet and enter the international waters of ‘moderate drinking’, where safe passage is not always clear. As already mentioned, discussion in the media about the risks - and even benefits - of alcohol is chaotic. Public health guidance can be vague, producing statements such as ‘there is no safe level of drinking’ without being clear exactly what this means, and this can come across as a touch puritanical. I have full sympathy with public health officials who have the Herculean task of continually having to encourage people to stop doing things they enjoy, but such statements are liable only to elicit a certain resentment at being made to feel guilty for enjoying one of life’s few remaining simple pleasures.
Furthermore, such statements are misleading, because there is no safe level of anything, with the exception of breathing perhaps. Certainly there is no safe level of sugar consumption, or driving, or stress due to working too much. Really, to say that there is ‘no safe level of drinking’ is a clever evasion, the statement least likely to land anyone in trouble, but it doesn’t really tell us anything or be of use to anybody who actually drinks. To this end I think it would be more realistic to adopt a ‘better drinking’ approach, as in; how to turn a potentially harmful habit into something that can be enjoyed, with minimal harm to your overall health. We will see that this is in fact entirely possible, but to help understand why it is helpful to look in a bit more detail at how alcohol is processed in the body.
Alcohol Metabolism
Among the many erroneous health beliefs that I used to entertain was that it was possible to sweat alcohol - or the remnants of it the next day - out of the body. Another was that if I drank enough water during a night out I would be able to dilute the alcohol in my bloodstream and slow its effects (true) and therefore pee it out before it could cause any harm (false). As it turns out, less than 5% of alcohol is excreted intact in urine, sweat or breath and little seems to alter this (though there is evidence that something called ‘isocapnic hyperventilation’ can increase ethanol clearance four-fold, which potentially hold some application in acute intoxication but seems practically challenging, not to mention unpleasant).
A more widespread myth that I often see online is that alcohol stays in the system for many months, even years. Like a lot of clickbait this is spurious but has a small grain of truth. A minuscule amount, less than 0.5%, of alcohol is processed via ‘non-oxidative’ metabolism, in which the alcohol molecule is incorporated into larger molecules called fatty acid ethyl esters (FAEEs) which do linger for a long time in the body. This seems to be more a product of binge drinking, and accumulation of FAEEs is implicated in pancreatitis. However, in moderate drinking the body uses a safer metabolic pathway, the same one that we evolved when our ape-like ancestors came down from the trees and started eating boozy fruit.
ADH and ALDH
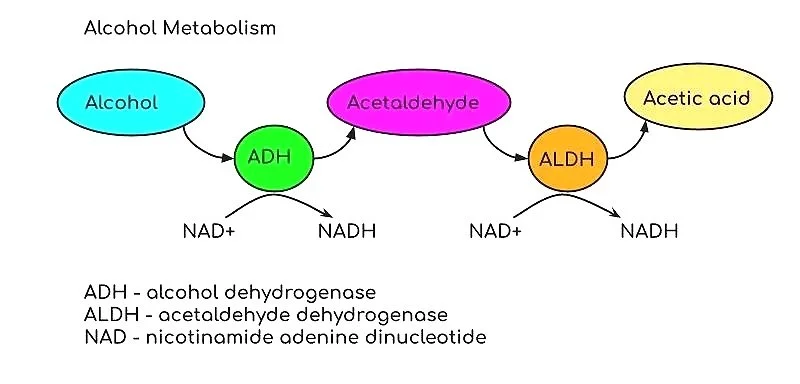
Around 95% of the alcohol we ingest is processed via oxidative metabolism. This involves two steps: conversion of alcohol to acetaldehyde, and then acetaldehyde to acetate, a.k.a acetic acid. Alcohol is broken down by the enzyme alcohol dehydrogenase (ADH) which is abundant in the upper GI tract and liver (where it comprises about 3% of the soluble protein). It breaks down alcohol with the ‘reduction’ of the molecule NAD+ to NADH.
Alcohol is broken down to acetaldehyde then acetic acid mainly in the gut and liver. Although the rate of alcohol elimination is roughly 1 unit per hour, factors such as food can have a significant effect on metabolism.
Other than it being a sugar, alcohol is non-toxic, as is acetate. It is the intermediary metabolite acetaldehyde that is chiefly responsible for the harmful physical effects associated with drinking (we’re ignoring behavioural consequences for now). Acetaldehyde is converted rapidly, within minutes, into acetate by the enzyme acetaldehyde dehydrogenase (ALDH) found primarily in the liver. Recent research has shown that up to 30% of acetaldehyde can be excreted by the liver in bile, which is the then processed by gut ALDH, so increased bile flow can also increase alcohol elimination rate (AER).
The Variants
Not everyone processes alcohol the same. Genetic variants can affect the expression of enzymes like ADH which lead to a faster breakdown of ethanol to acetaldehyde. Such a variant is common in people from east Asia and around 25% of people of Jewish descent. Perhaps better known is the variant of ALDH - ALDH2*2 - which is common in certain Asian populations (Han Chinese, Korean and Japanese) and is virtually inactive, leading to a build-up of acetaldehyde after drinking, resulting in the notorious ‘flush reaction’, involving headache, nausea and increased heart rate and which can be severe enough to constitute a functional ‘allergy’ to alcohol. (Perhaps as some consolation, the incidence of alcoholic cirrhosis is reduced by 70% in ALDH2*2 carriers.)
It is also possible to intentionally disable ALDH with certain medications like disulfram, sometimes used by heavy drinkers to make themselves functionally allergic to alcohol, and certain antibiotics like metronidazole which knock out ALDH. There doesn’t seem to be a way to significantly increase ALDH activity, though there is a drug called metadoxine which seems to be able to do this to some extent. In any case ALDH works quickly enough, but the ‘rate-limiting factor’ is the availability of the enzyme - the liver only has so much ALDH at any one time and can’t speed up supply. The enzymes reach a saturation point after less than one drink and after then it is very much a case of ‘one-in, one out’ when it comes to alcohol metabolism, that is to say, alcohol is processed at the same rate regardless of how much is in the bloodstream, a phenomenon known as zero-order kinetics.
Other Pathways
Not all alcohol is cleared via the ADH-ALDH double act. In the brain alcohol is metabolised via an enzyme called catalyse. In heavier drinking the liver recruits another class of enzymes called the cytochrome-P450s (CYP450) to deal with the excess. CYP450s are the workhorse of the body’s detox system, involved in the breakdown, among other things, of medications such as opioids like morphine or codeine, non-steroidal anti-inflammatories (NSAIDs) and most anti-depressants like SSRIs, which is why, in general it is safe to drink – within reason - while taking these medications as they are not competing for the same enzyme - though it’s worth noting that alcohol and NSAIDs can both cause gastric irritation.
Normally CYP450 plays a minor role in the clearance of alcohol but with chronic, heavy drinking the body increasingly relies on CYP450s which, when metabolising alcohol, produce more reactive oxygen species (ROS) which cause tissue damage, mainly in the liver. When we talk about ‘oxidative stress’ we are chiefly talking about the effects of the (not-so-friendly) ROS. Anti-oxidants can help mitigate the effects of ROS, and some research has shown antioxidants such as S-AME, NAC, folic acid and vitamin C can help protect liver cells.
The toxicity of acetaldehyde is mainly in that it provokes inflammatory molecules and interacts with certain proteins to form adducts which interfere with normal cell production. For example, adducts can form on the surface of red blood cells, causing them to enlarge (called macrocytosis), or in those involved in iron storage, leading to high iron levels, both of which are often seen in heavy drinkers. Adducts can also form with collagen proteins on the skin or in certain cells in the liver and even the brain. Reducing the toxic byproducts of acetaldehyde seems to be really a matter of both reducing acetaldehyde build-up and increasing its clearance. The question naturally arises of how.
Food: The Drinker’s Friend
The most reliable way to do this is with food. We’ve seen how food can increase first-pass metabolism by as much as 50%. Eating also naturally slows down the rate of alcohol ingestion - we tend to drink a lot slower with a plate of tapas or other nibbles in front of us. Interestingly, food also increases the rate of elimination of alcohol and acetaldehyde when already in the systemic circulation. Having something to eat increases ethanol elimination by as much as 33-50%. Studies vary on which type of food is better at this, but one showed that a varied meal of fat, protein and carbohydrates led to an increased elimination rate of 45%. Fructose, normally a dietary villain, seems especially effective at speeding alcohol elimination, perhaps accounting for some people craving sugary food after drinking, or the custom apparently common in Russia of eating fruit while drinking. The ‘fructose effect’ is chiefly due to fructose metabolism converting NADH back to NAD+, which is then used by ADH and ALDH. Other ways in which eating is thought to speed up ethanol elimination are that food increases the activity of ADH, increases blood flow to the liver and promotes bile flow.
The Hangover
A lot has been written about hangovers. No decent work of literature is complete without someone at some point experiencing a catastrophic hangover. There is also a wealth of articles about how to treat hangovers, ranging from the standard ‘hydrate and rest’ advice to more colourful formulations like Anthony Bourdain’s tempting ‘aspirin, cold coca cola, a joint and spicy Szechuan beef.’ Hangovers are due to a constellation of insults to the body. Causes include gastric irritation and sometimes a stomach that refuses to empty thanks to pylorospasm, at times culminating in an unfortunate expulsion the other way*. The dehydration is thanks to alcohol inhibiting vasopressin, or anti-diuretic hormone (ADH). ADH tells the kidneys to reabsorb water back into the body, so its inhibition leads to water and salt loss in urine. Poor sleep results from alcohol inhibiting REM sleep and also a rebound of adrenaline levels, usually around 2 in the morning, often combined with the diuretic effect. Then there is general inflammation triggered by oxidative stress from acetaldehyde production and of course the aforementioned anxiety resulting from too much glutamate and too little GABA in the nervous system. Fortunately in most cases the physical effects wear off by 24 hours.
With regards to what drinks are worse for hangovers, generally it is a matter of quantity rather than quality, but drinks rich in congeners, which add complexity and flavour, and are found in wine or whisky, can result in especially severe hangovers. Why? Certain congeners like quercetin-3-gluconaride found in wine inhibit ALDH, leading to accumulation of our old fried acetaldehyde. On the other hand wine is also rich in flavinoids which have anti-oxidant properties.
* Studies have shown that alcohol concentrations above 30% tend to cause the pyloric sphincter at the exit of the stomach to clench shut, perhaps sensing a potential toxin.
How Much Is Safe?
The harms of heavy, chronic drinking are well established and the consequences are usually obvious both mentally and physically. However, when it comes to light-to-moderate drinking the long-term risks are not that easy to determine because this type of drinking doesn’t usually produce conditions like liver cirrhosis. For this reason research tends to focus on health outcomes like cardiovascular disease or dementia and then compares a population of drinkers to non-drinkers in a retrospective study; that is, a study that takes a group and looks back over the past decades and comparing rates of disease among self-reported drinkers and abstainers. Researchers then try to pick apart the data, trying to remove ‘confounding factors’ such as economic status, to tell as far as possible if alcohol is associated with a higher risk of developing, say, dementia or having a heart attack, compared to not drinking.
How Much Is in a Drink?
Scientists tend to measure alcohol in grams. In the US a standard drink contains 14g of ethanol which is equivalent to a 12 oz can (354mL) of 5% ABV beer, a 5oz (148mL) glass of 12% wine, or 1.5oz (44mL) spirit at 40%. In the UK we tend to use the unit, which contains 8g ethanol. Calculating how many units you’ve drunk is fairly straightforward:
Unit/s = % ABV x mL divided by 1000
So a 330mL can of 5% beer is 5 x 330 / 1000 = 1.65 units, or;
A pint of 4% beer is 4 x 568 / 1000 = 2.3 units
Of note, there is no fixed ‘standard drink’. In the UK it is usually 1.25 units. In the US it’s 1.75 units. To make matters more confusing it is not always clear which a study is using, so for the sake of convenience I am generalising a drink to around 1.5 units, which is roughly a small can of beer or glass of wine.
The J Shaped Curve
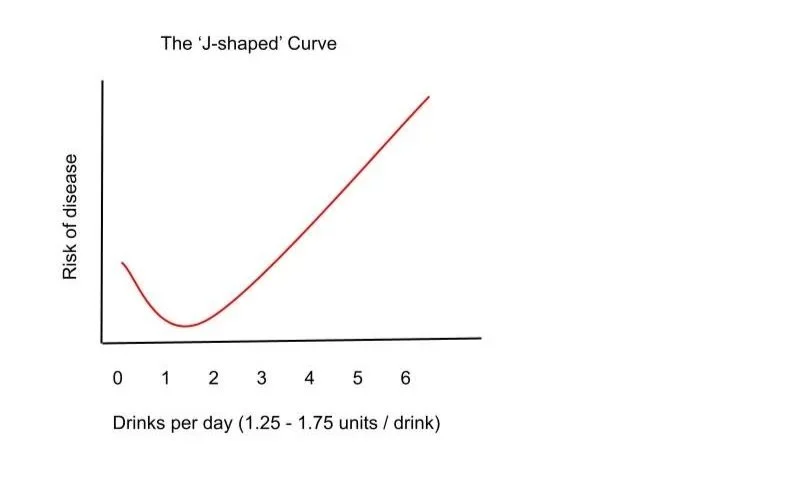
The media obsession with the hazards of moderate drinking are, of course, chiefly driven by the need to get a target audience clicking on articles. Anything that provokes anxiety is a tried and tested way to do this, and there is also a lot of mileage to be had out of recycling contradictory messages. So we are informed that moderate drinking is protective of health and then also that there is ‘no safe level of drinking’. Which is it? Most large-scale studies and meta-analyses over the past few decades show similar findings; that 1-3 drinks a day carries a low risk for cardiovascular events like strokes or heart attacks, as well as metabolic disease like diabetes and neurological conditions like dementia. After 3 drinks a day the risk starts to increase and after 4-5 per day this rises further. Interestingly - and this seems to be the cause of much controversy - complete abstinence tends to show a slightly increased risk of these diseases, leading to the classic ‘J-shaped' pattern.
Many large scale studies over the past two decades show a slightly reduced risk among light to moderate drinkers compared to non-drinkers for diseases like heart attacks, type 2 diabetes and strokes. The risk then increases.
There is no clear idea why this should be so. Are moderate drinkers more relaxed? Does wine or beer contain protective compounds? Do moderate drinkers live otherwise healthier lifestyles? Do they exercise more? Are teetotallers more likely to have other health problems? Periodically research will attempt to debunk this J-shaped model, leading to the ‘no safe level of drinking’ pieces. These often use very sophisticated genetic modelling and show that drink doesn’t actually prevent disease - effectively flattening the first part of the ‘J’. The debate is ongoing, but perhaps it may not be that important. For one, I can’t imagine any non-drinkers will start drinking to reduce their risk. Also, for most light-to-moderate drinkers their main concern is whether drinking is going to harm them long-term, and the studies consistently seem to say the same thing: probably not.
Two Types of Risk
A crucial distinction with any study that looks at risk is between relative and absolute risk. Absolute risk can be thought of as the ‘real world risk’, taking into account the overall prevalence of a given health problem. For example, a study might say that doing X doubles your risk of D. In other words X doubles your risk relative to not doing X. However if D only occurs in one in a million people, the absolute risk has only risen from 1 to 2 in a million.
As an illustration, a 2018 study in the Lancet into the global impact of alcohol consumption, showed a steadily increasing relative risk of alcohol-related health problems after just one drink (1.25 units) a day and led to the conclusion that there was ‘no safe level of drinking’. However the scientists behind the study then released their findings using absolute risk and this gave the findings a different complexion: with 1 drink a day the absolute risk rises only 0.5%
“…meaning 914 in 100,000 15-95 year-olds would develop a condition in one year if they did not drink.…and this goes up to 918 in people who have a drink a day.”
This goes up to a 7% absolute risk for people who drink two alcoholic drinks a day (977 people in 100,000 developing an alcohol related health problem) and goes up to 1252 people in 100,000 with 5 drinks a day. Statistics expert David Speigelhalter puts this into further context; ‘upon closer inspection (the data) still shows 1600 people would need to drink 32 bottles of gin in a year for one person to develop an alcohol related health issue.’*
In any case, most people are aware on some level when they are drinking too much. Getting from here to a place where one is no longer dependent on, or anxious about, drinking can seem like a daunting prospect, but an important step is to take away questions of moral judgement. The fact is that we have evolved to seek pleasurable things, or things which take away the stress, boredom, worry and irritations of life, and alcohol not only does this effectively and quickly but usually tastes nice too, and is often associated with other enjoyable things like food and company. In this respect it is perhaps better to view alcohol as a medicine, with its own risks and benefits, and find a level of risk one is comfortable with. For some heavy drinkers - the oblivion-destructive drinkers - they have little choice but to stop, but for the lighter, less dangerous drinkers complete sobriety may not be realistic or even that much better for them. Of course, there is a lot to be said for being sober, or periods of abstinence, and it can feel very satisfying to know that you don’t need to drink, that it really is a choice. It’s also refreshing to wake up relatively clear headed. An ‘alcohol-fast’ of the Dry-January type may not quite bring the life-changing clarity one hopes for, but at least it clears the skin up a bit. All of which, dare I say, we can look forward to after the festive season.
Below are a selection of studies which support the hypothesis that light-to-moderate drinking can confer some reduction in risk of certain diseases, or is at least relatively okay in terms of health
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(18)31310-2/fulltexthttps://www.bmj.com/content/342/bmj.d671
Recent advances in alcohol metabolism: from the gut to the brain, MR Goldman, M Molina-Castro et al. Physiol Rev. 2024
GABAa receptors and alcohol, I A Lobo & R A Harris, Pharmacol Biochem Behav. 200
https://alcoholchange.org.uk/alcohol-facts/fact-sheets/drinking-trends-in-the-uk